What Is The Evidence For Specific Management And Treatment Recommendations
Crone, Am, Stewart, EJ, Wojnarowska, Powell, SM. âAetiological factors in vulvar dermatitisâ. J Eur Acad Dermatol Venereol. vol. 14. 2000. pp. 181-6.
Goldstein, AT, Thaci, D, Luger, T. âTopical calcineurin inhibitors for the treatment of vulvar dermatosesâ. Eur J Obstet Gynecol Reprod Biol. vol. 146. 2009. pp. 22-9.
Stewart, KMA. âClinical care of vulvar pruritus, with emphasis on one common cause, lichen simplex chronicusâ. Dermatol Clin. vol. 28. 2010. pp. 669-80.
Stockdale, CK, Boardman, LA. âBenign Disorders of the Vulva. In Precis: an update in obstetrics and gynecologyâ. American College of Obstetricians and Gynecologists. 2011.
Copyright © 2017, 2013 Decision Support in Medicine, LLC. All rights reserved.
No sponsor or advertiser has participated in, approved or paid for the content provided by Decision Support in Medicine LLC. The Licensed Content is the property of and copyrighted by DSM.
What Causes Neurodermatitis
The underlying cause of neurodermatitis is unknown. However, it has been observed that the itch can start during times of extreme stress, anxiety, emotional trauma or depression. The itching sometimes continues even after the mental stress eases or stops.
Other possible neurodermatitis triggers include:
- Nerve injuries.
- Wearing tight clothing, especially if the material is a synthetic fiber, like polyester or rayon. These factors can cause sensitive skin to overreact and itch.
- Other skin diseases. Neurodermatitis sometimes happens as a result of eczema and psoriasis.
Groin Or Vaginal Infection
Washing tips: Clean the area in warm water at least twice a day. Pat dry carefully and then apply any cream you have been given by your doctor or pharmacist.
Wash your hands before and after cleaning to prevent the spread of the infection. Also, do not share your face cloth or towel with others.
Creams: If you are using intravaginal creams or pessaries, youâll need to use menstrual pads rather than tampons.
Clothing: Change underwear daily and wear loose-fitting pants.
Pain relief: If you are in pain, get advice on medicines you can take.
You May Like: Baby Has Eczema All Over Body
Also Check: What Emollients Are Good For Eczema
The Problem With Self
When vaginal or vulvar itching occurs, women usually assume it’s a yeast infection and treat it with an over-the-counter antifungal cream. Often this does the trick, but not always. Instead, the cause of the symptoms might be dry skin, a sexually transmitted disease or bacterial infection, a less common strain of yeast that required special medication, or irritation by and allergic reactions to common products such as soaps, creams, and lotions.
If yeast isn’t the problem, an antifungal cream isn’t the solution. And if your skin is already irritated, you may exacerbate the problem by introducing preservatives and other ingredients contained in many antifungal remedies. That’s why it’s important to see your gynecologist or dermatologist if a problem persists after you’ve tried a standard antifungal cream.
Another common response of women faced with a vaginal discharge or itch is to wash the vulvar skin vigorously, on the assumption that this will disinfect the area or remove irritants. But aggressive cleansing can add to the irritation. Until the problem is diagnosed, it’s best to follow a gentle skin care routine . In fact, gentle cleansing applies whether you have a vulvar skin condition or not: Wash the area gently with your fingertips or a soft cloth and pat dry with a soft towel. Don’t use a rough washcloth, and don’t rub.
How Can You Ease The Pain From Genital Eczema
To help relieve discomfort in the area, you can use a cold compress. Over-the-counter pain relievers such as ibuprofen or acetaminophen may also be effective for reducing burning, pain, and inflammation in the genital area. In some cases, antihistamines can reduce inflammation. Some specific OTC antihistamines that you can try include Benadryl, Zyrtec, Claritin, and Allegra.
Don’t Miss: Best Treatment For Eczema On Arms
How Do You Treat Itching In A Mans Private Parts
Generally, itching or irritation in the private parts goes away on its own with simple measures, such as:
- Washing the affected area with clean and warm water
- Keeping the area dry
- Wearing well-fitting and breathable undergarments
If you are obese or overweight, reducing your weight may also help control the infection.
If the itching keeps recurring, consult a doctor. Treatment will target the cause of infection and your doctor may prescribe medication to control the itching. Your doctor may even advise you to avoid using any personal care products in the genital area that might aggravate the itching. Depending on the cause of the infection, they may prescribe antifungal medications, antiviral medications or antibiotics.
Genital itching may also be aggravated by diabetes and other conditions that weaken immunity. In the case of diabetes, the doctor will prescribe medications and suggest lifestyle changes to control your blood sugar levels. Phototherapy may be used if the itching is due to lichen sclerosus. Other underlying conditions, such as eczema or psoriasis, will also be addressed.
Getting A Diagnosis For Vulva Skin Conditions
Getting a diagnosis for vulva skin conditions
Vulvar skin conditions are highly treatable, but the treatment depends on the specific cause. And identifying the underlying diagnosis can be very challenging.
Tell your clinician about any other past or present medical conditions and any skin problems elsewhere on your body. For example, psoriasis anywhere on the body raises the risk of a vulvar condition known as lichen sclerosus. Crohn’s disease, a chronic inflammatory intestinal disease, may cause abscesses or draining fistulas in the vulvar area, and vulvar skin problems are often one of its early symptoms. A mouth condition called lichen planus is another cause of vulvovaginal problems. Long-term treatment with oral steroids, immune suppressants, or antibiotics can affect vulvar skin and raise the risk infection.
Your clinician will want to know how you care for your vulvar skin, which can help identify possible sources of irritation. Even if you can’t pinpoint a change, that doesn’t mean your standard routine isn’t the culprit. Sometimes vulvar problems are the cumulative effect of long-term practices.
It’s often what you’ve done day after day, year after year, that causes the problem. If you wear abrasive clothing and engage in abrasive activities like bicycling or spinning class and wear tight workout clothes that expose your vulva to sweat or to detergent or soap residue, eventually it might catch up with you.
Read Also: What Causes Baby Eczema Flare Ups
What Are The Treatments For Vulvar Dermatitis
The treatment for vulvar dermatitis will depend on the cause.
In the case of contact dermatitis or an allergic reaction, a person may need to change their soaps or detergents to avoid irritants.
If an infection is responsible, the doctor might prescribe medications such as oral antibiotics or topical creams.
Although there is for atopic dermatitis, many treatments are available. Doctors may prescribe one or more of the following treatments to manage the symptoms and prevent complications:
- moisturizing creams
- topical treatments, such as steroid creams
- oral or injectable medications, for moderate to severe eczema
The severity of a personâs symptoms and the amount of their body that eczema affects will determine the treatment plan. People may need to try more than one treatment.
Alongside treatment, lifestyle changes may help reduce the symptoms of vulvar dermatitis.
Discussion Of Terms Related To Eczematous And Lichenified Diseases
Nomenclature regarding the eczematous and lichenified diseases is particularly confusing and controversial. For this reason, our committee thought that it would be informative for users of the 2011 ISSVD classification of vulvar dermatological disorders to indicate how we believe these terms should be defined and used.
Eczema
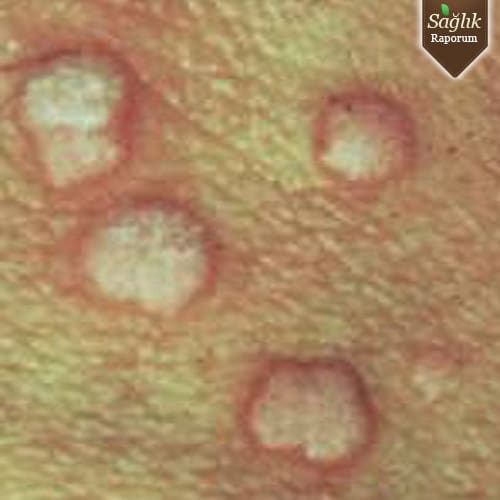
The term eczema classically refers to a group of inflammatory diseases that are clinically characterized by the presence of pruritic, poorly marginated red plaques with minor evidence of microvesiculation and/or, more frequently, subsequent surface disruption . Histologically, the eczematous diseases are characterized by a “spongiotic pattern” . Chronic forms of eczematous disease may develop scaling and/or lichenification. The term dermatitis is used as a synonym for eczema or is misused as a nonspecific term to describe any inflammatory skin condition.
Surface Disruption
Visible evidence of surface disruption includes one or more of the following: weeping, crusting, microvesiculation, fissuring in the folds, and erosions most often occurring as a result of excoriation.
Lichenification
Lichen Simplex Chronicus
Atopic Dermatitis
Publication History This article was presented at the XXI World Congress of the International Society for the Study of Vulvovaginal Disease, held in Paris, France, on September 3 to 8, 2011.
J Low Genit Tract Dis. 2012 16:339-344. © 2012 Lippincott Williams & Wilkins
Also Check: Organic Eczema Cream For Toddlers
What Questions Should I Ask My Healthcare Provider About Itchy Genitals
- Whatâs causing my itchy genitals?
- Whatâs the best treatment?
- Are there any over-the-counter products I should use?
- What can I do at home to manage my itchy genitals?
- How can I prevent itchy genitals?
- What products should I avoid?
A note from Cleveland Clinic
You donât have to just live with itchy genitals. There are effective treatments to relieve or even eliminate your symptoms. See your healthcare provider for help and be sure to take your medications as directed. Itchy genitals shouldnât interfere with your quality of life. Do your best not to scratch so that you donât make your itchiness worse!
Last reviewed by a Cleveland Clinic medical professional on 01/07/2021.
References
Is It An Sti Or Genital Eczema
Although the symptoms of genital eczema are similar to those of some sexually transmitted infections , there are some signs that an infection is to blame for the itching and irritation. If you notice any odor, discharge, bleeding, or signs of infection such as a fever or body aches, its more likely that you have an STI, not genital eczema.
You May Like: Best Thing For Eczema On Eyelids
Eczema In Genital Area Causes: Symptoms And Natural Remedies
Eczema in genital area is most embarrassing skin ailment for both men and women, sometime affecting sexual activity and interpersonal relationship. Due to its anatomical site many people feel awkward to consult their doctor. But without feeling ashamed, you have to talk with your doctor so that the underlying skin problem can be resolved early.
Just like anywhere else, eczema in genital region causes intense itching, soreness, watery discharge, and irritation. It becomes difficult for a person to resist scratching. Eczematous skin lesion can affect the skin near genitals, skin between the two buttocks, around the pubic mound, skin fold in groin, perianal area in women.
Besides conventional ointments and medicines, there are several home remedies that are effective in treating this discomforting condition.
How To Treat Eczema In The Genital Region

Ive experienced irritating skin in the genital region for a good part of my life. Eczema was most common and was extremely uncomfortable. I know the pain if you are going through it also. With this post, I hope to help you heal it and prevent it from coming back for life. How to treat eczema in the genital region?
To treat eczema in the genital region, first, see a doctor who will confirm whether it is eczema or a different issue. The doctor should then prescribe a mild topical steroid or emollient to reduce inflammation. Shower or bathe each morning or night, pat dry after, apply the topical steroid leaving no excess.
Theres much more to take into consideration when treating eczema in the genital area. For example, do not overuse steroid cream or ointment to avoid thinning the skin. The skin in the genital region can be quite sensitive and thin, so you dont want to use a strong steroid cream.
Your doctor will prescribe a mild dose as the genital region is so sensitive. Be wary of self-treating. And watch out for the many, many harmful everyday products that may be causing the inflamed skin.
Read on to learn more about how to treat eczema in the genital region and prevent it from recurring!
Don’t Miss: Is Eczema Itchy At Night
Herpes Simplex Virus Type 1
HSV-1 commonly causes cold sores, known as oral herpes. HSV-1 is very contagious.
According to the World Health Organization , about 67% of people under the age of 50 have HSV-1, globally.
HSV-1 can spread through sexual contact from the mouth to the genitals, but it is not necessarily a sexually transmitted infection . Many people get HSV-1 through nonsexual contact, including kissing or sharing personal items, such as lip balm or utensils.
Symptoms Of Eczema In Genital Area
Many people feel too embarrassing discussing symptoms pertaining to their genital region this also includes eczematous skin lesions around genital area. One of the most common symptoms is intense itching in and around the genital region. Person cannot resist scratching although it may feel embarrassing especially in front of people.
The affected skin becomes red and sore.
In some cases the skin is dry and scaly instead of watery and oozing. Dark colored rough skin patches may be present.
Don’t Miss: Does Eczema Ever Go Away
Types Of Genital Eczema
There are four types of eczema that could develop in the genital area:
- Atopic dermatitis: This type of eczema presents as an itchy and scaly rash. It is due to a reaction in the skin, which leads to ongoing itching, swelling, and redness. People with atopic dermatitis may be more sensitive because their skin lacks specific proteins in the skin barrier, the top layer of the skin that protects it from pathogens.
- Seborrheic dermatitis: It causes itchy red patches and greasy scales on your skin, along with white or yellow crusty or powdery flakes on your scalp. Although this type of eczema is more common on the scalp, it can also affect other parts of the body that have a lot of oil glands, including the groin.
- Allergic contact dermatitis:When the genital area is exposed to an allergen, it can lead to the development of eczema in the area. It typically occurs 48 to 72 hours after exposure to the allergen.
- Irritant contact dermatitis: Irritant contact dermatitis occurs when chemicals or physical agents damage the surface of the skin faster than the skin can repair the damage. Irritants remove oils and moisture from the skin’s outer layer, allowing chemical irritants to penetrate more deeply and cause further damage.
There are different types of genital eczema depending on which part it affects:
- Scaly or leathery patches of skin
- Swelling or irritation
What Can I Do To Improve My Situation
Make sure that you are diligent with your application. Vaginal eczema is different from any other kind of eczema because recovery period can take up to 1 months , simply because the vulva and the vaginal are in an environment that can harbor bacteria easily.
Here are a few things you can do to improve your vaginas struggle with eczema:
Just make sure you use a very low dose type due to the extremely sensitive nature of vulval and vaginal skin. An application of the steroid ointment once or twice per day is acceptable and have been reported to not cause any side effects as long as the usage is sparse.
You May Like: How Do I Know I Have Eczema
How To Spot Early Symptoms Of Eczema Herpeticum
The first signs of eczema herpeticum occur about 5 to 12 days after exposure to HSV, says the AAD. At that point, it can be easy to think that changes in the skin are simply a particularly bad flare-up of eczema.
However, symptoms of eczema herpeticum which include painful red, purple, or black blisters tend to be more dramatic in appearance than eczema, says the NEA.
These blisters typically occur on the face and neck, but they can appear anywhere on the body where there is eczema and the skin has been in contact with the herpes virus.
In addition to a painful, blistery rash, eczema herpeticum can cause more general body-wide effects, says Sruthi Renati, MD, an assistant professor of dermatology at the University of MichiganMichigan Medicine in Ann Arbor.
Some patients develop high fevers, a general feeling of discomfort or feeling unwell, and enlarged lymph nodes, she explains. These symptoms often start as the blisters are appearing.
Due to the potential for severe complications, you should call your doctor or dermatologist right away if you or a family member who has eczema develop any of the following symptoms:
- A cluster of small, itchy, painful blisters
- Blisters that are around the same size and have a punched-out look
- Blisters that are red, purple, or black
- Crust that forms over older blisters
- Blisters that ooze pus when broken
- A cold sore above the upper lip
- High fever and chills
Home Remedies And Care Tips
In addition to your medication, there are some things you can do at home to keep yourself comfortable. Always talk to your doctor before you begin any at-home treatments like:
Baking soda soaks. You can soak in lukewarm bath water with 4 to 5 tablespoons of baking soda to help soothe your vulvar irritation. Do this one to three times a day for 10 minutes.
Gold Bond or Zeasorb Powder. You can sprinkle these on your underwear to control dampness. Donât use other forms of powder or cornstarch.
To get the best treatment outcome, follow these care instructions:
- Donât wash your vaginal area more than once a day. Only use cool water with or without a mild soap.
- Use unscented sanitary pads or tampons during your period.
- Donât have sex until you feel better.
- Try sleeping without any underwear.
- Wear looser clothing. Stay away from nylon or other fabrics that hold in heat and moisture.
Show Sources
Don’t Miss: What Not To Eat When You Have Eczema
Vulvar Skin Conditions And Their Treatment
Several vulvar skin conditions are familiar from other areas of the body but may be difficult to recognize when they appear on the vulva. These include the following:
Eczema. This inflammatory skin condition disrupts the skin’s surface, causing red patches and thin cracks, weeping, and crust formation. On the vulva, crusts are less likely, but eczema may initiate a cycle of vulvar itching and scratching that leads to lichen simplex chronicus thickened and intensely itchy skin. If eczema affects an area of the vulva called the vestibule, it may cause stinging and burning. Sometimes eczema appears in early childhood and its cause is unknown. More often, it begins with exposure to an irritant or allergen .
|
Many things can cause an allergic reaction or irritate vulvar skin. Here are some of the leading suspects: Irritants
Allergens
Adapted from The V Book, by Elizabeth G. Stewart, M.D., and Paula Spencer . |
To diagnose vulvar eczema, the clinician will ask about your symptoms your history of eczema, allergy, and related conditions your vulvar cleansing habits and any products the vulva has been exposed to. During the exam, she or he will look for redness, scaling, cracking, and thickening.