Q : How Does Eczema Affect People Of Different Ages
Eczema is a chronic health problem that affects people of all ages, but is most common in babies :
- Infantile eczema occurs in around 20% of children under two years of age, and usually starts in the first six months of life. Infantile eczema usually improves significantly between the ages of two to five years.
- Childhood eczema may follow infantile eczema, or start from two to four years of age. Rashes and dryness are usually found in the creases of the elbows, behind the knees, across the ankles and may also involve the face, ears and neck. This form of eczema usually improves with age.
- Adult eczema is similar to that of older children with areas of very dry, itchy, reddened skin at the elbow creases, wrists, neck, ankles and behind the knees. It can cause rough, hard and thickened skin, which may also have weeping areas. Although eczema tends to improve in midlife, and is unusual in elderly people, it can occur at any age.
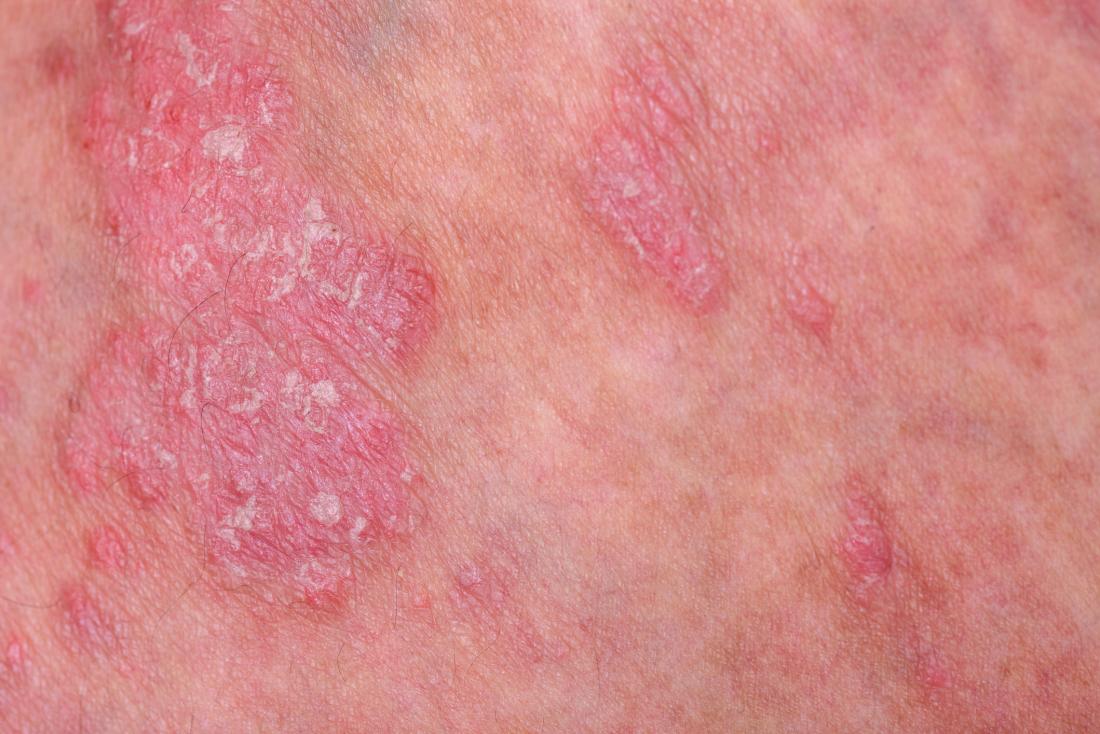
How Is Psoriasis Diagnosed And Treated
Psoriasis often has a typical appearance that a primary care doctor can recognize, but it can be confused with other skin diseases , so a dermatologist is often the best doctor to diagnose it. The treatment of psoriasis usually depends on how much skin is affected, how bad the disease is , or the location . Treatments range from creams and ointments applied to the affected areas to ultraviolet light therapy to drugs . Many people who have psoriasis also have serious health conditions such as diabetes, heart disease, and depression. Some people with psoriasis also have an inflammatory condition which affects their joints, called psoriatic arthritis.
Psoriatic arthritis has many of the same symptoms as other types of arthritis, so a rheumatologist is often the best doctor to diagnose it. The treatment of psoriatic arthritis usually involves the use of drugs .
Psoriatic disease may be treated with drugs or a combination of drugs and creams or ointments.
What Can Go Wrong With Your Immune System
When your immune system doesn’t work the way it should, it is called an immune system disorder. You may:
-
Be born with a weak immune system. This is called primary immune deficiency.
-
Get a disease that weakens your immune system. This is called acquired immune deficiency.
-
Have an immune system that is too active. This may happen with an allergic reaction.
-
Have an immune system that turns against you. This is called autoimmune disease.
Don’t Miss: What Percent Of The Population Has Eczema
What Questions Should I Ask My Healthcare Provider About Eczema
- How can you tell that I have eczema?
- If I dont have eczema, what other skin condition might I have?
- Is there a specific brand of moisturizer that you recommend?
- Is there a prescription cream that you can prescribe?
- How often should I see a dermatologist regarding my eczema?
- What soaps, lotions, makeup, etc. should I avoid?
- What medications do you recommend?
- What at-home treatments do you recommend?
A note from Cleveland Clinic
Eczema is very normal, very common, and very, very uncomfortable. It can affect your quality of life. At its worse it can keep you from sleeping, distract you and make you feel self-conscious in public. See your dermatologist or other healthcare provider as soon as you start to see signs of it. Explore at-home remedies and prescribed treatments.
Youre not alone! 15% to 20% of people experience eczema or another type of dermatitis at some point in their lives.
The Trick To Identifying Eczema Triggers

Patch testing is a tool many doctors use to diagnose potential eczema triggers. In this test, allergists like Wein apply adhesive strips or patches to an eczema-free area of the back. The patches contain substances that are believed to cause irritation in people with eczema.
After 48 hours, the doctor removes the patches and inspects the skin for reactions. After two more days, the doctor looks at the patch sites for signs of inflammation. If there is inflammation, the allergy to a particular substance is confirmed.
Most scientific evidence regarding trigger factors in AD relates to dietary exclusions or house dust mite avoidance strategies, Wein said. There is little consistency across studies in the type of diet evaluated, and indications for special diets were not always made clear. It is also unclear what role factors such as stress, humidity or extremes of temperature have in causing flaresjust that these factors should be avoided where possible.
Heeley knows firsthand the frustration that comes when elimination diets fail to identify triggers. He wonders if the stress of trying to identify triggers might contribute to his flare-ups.
Maybe I need to tone down my stress level and think more calmly about tackling the problem, he admitted. I just knew that it had something to do with food and my digestive tract. I thought I tried all of the elimination diets, but I couldnt find anything that correlated.
Don’t Miss: What Vitamins Are Good For Eczema
The Inherited Barrier Defect
There is emerging evidence that inflammation in atopic dermatitis is associated with immune-mediated and inherited abnormalities in the skin barrier. This barrier failure causes increased permeability of the skin and reduces its antimicrobial function.
The main inherited abnormality causing disordered barrier function is filaggrin expression. Filaggrins are filament-associated proteins which bind to keratin fibres in the epidermal cells. The gene for filaggrin resides on chromosome 1 . This gene was first identified as the gene involved in ichthyosis vulgaris. Abnormal filaggrin is associated with early-onset, severe and persistent atopic dermatitis.
It is postulated that the loss of filaggrin results in:
- Corneocyte deformation , which disrupts the organisation of the extracellular lipid the lamellar bilayers.
- A reduction in natural moisturising factors, which include metabolites of pro-filaggrin.
- An increase in skin pH which encourages serine proteaseactivity these are enzymes which digest lipid-processing enzymes and the proteins that hold epidermal cells together. Serine proteases also generate active cytokines like IL-1a and Il-1beta and promote skin inflammation.
Proteins under investigation in atopic eczema include structural compounds, such as hornerin, cornulin, claudin 1/23 and ceramides, enzymes, such as kallikrein and serine peptidases.
Is Atopic Dermatitis An Autoimmune Disease
The American Academy of Dermatology Association states that is a common form of eczema that does not have a single cause. Researchers think AD develops due to a combination of genetics, a sensitive immune system, and environmental factors that trigger the symptoms. Some evidence suggests that autoimmunity may also drive it.
Dermatologists believe that people with AD have a genetic trait that means their skin loses moisture too quickly, causing gaps in the skin barrier. This can lead to dry, less well-protected skin.
This alone is not always enough to cause AD. Other factors that may put people predisposed to the condition at risk of developing it include:
- living somewhere that is cold and damp for at least some of the year
- exposure to pollution and tobacco smoke
Autoimmunity may also contribute to AD. The authors of a 2021 study suggest that AD may start as an allergic response before progressing to an autoimmune response. They argue that this may be what causes chronic inflammation and relapses.
A large 2021 population-based study also found higher AD rates in people with one or more autoimmune condition, particularly those that affect the skin and digestive tract. This suggests one may increase the risk of, or cause, the other.
However, more research on how AD develops is necessary to confirm that it is an autoimmune disease, and if so, what treatments might help.
Also Check: Can Eczema Go Away Without Treatment
A Natural Approach To Eczema
At the Eczema Life Clinic in Sydney we see a lot of new eczema patients with symptoms such as loss of hair and eyebrows, cracks at the corners of their mouth, insomnia, itchy skin and chronic dry and flaking skin and these are common nutritional deficiency signs, that are easily reversed with the right supplementation.
Best nutrients for eczema
- Calcium carbonate supplementation can improve sleep as calcium deficiency is a common cause of insomnia. While calcium citrate may worsen eczema, if you are sensitive to citric acid, calcium carbonate is a well-tolerated option. Calcium carbonate is also a salicylate sensitively remedy.
- Hair loss and cracked corners of the mouth are typical B vitamin deficiency signs, however high dose B vitamins can cause insomnia and deficiencies in other B vitamins so only take the RDI amounts .
- Zinc is an important nutrient for eczema and the best form is zinc gluconate as it has shown to benefit seborrheic dermatitis and eczema.
- Zinc is stored in the liver so take only the RDI amount: 8 to 14 mg for adults, and 3 to 7mg for children.
- Vegan omega-3 from algae to increase EPA levels in the blood, as EPA is anti-inflammatory.
You may have found supplementation has not helped your eczema and here are some possible reasons:
Supplement ingredients to avoid if you have eczema
These are common mistakes people make when trying supplements for their eczema.
What Is Dermatitis Herpetiformis
If your skin feels extremely itchy or starts to blister after you eat or drink products with gluten , you may have dermatitis herpetiformis or Duhrings disease, a chronic skin condition. The underlying cause of this gluten rash is usually celiac disease, an immune disease where ingesting gluten will damage your small intestine.
When people with celiac disease eat or drink gluten, their intestine produces the antibody immunoglobulin A antibodies against certain enzymes that deposit in the skin. This causes white blood cells to attack your skin. As a result of this abnormal immune response to gluten, a bad skin reaction emerges.
Unlike many autoimmune diseases, the cause of DH is not a mystery. Since we know that gluten is a trigger, it allows us to use more targeted treatment. Our dermatologists at University of Utah Health can properly treat you for DH to help improve your symptoms and keep flare-ups at bay.
Recommended Reading: How To Treat Ear Eczema
How Allergies Asthma And Eczema Interact
Eczema flare-ups, asthmas attacks, and allergic reactions can all occur at the same time when you are exposed to a trigger. Triggers cause your immune system to overreact to a substance that it views as foreign. Each person’s triggers are different, but there are several types that can cause both your eczema and asthma symptoms to increase, including:
While there’s no cure for eczema or asthma, there are several ways symptoms can be managed.
Over-the-counter medications can treat symptoms caused by both eczema and asthma.
- Anti-inflammatory and pain-relieving medications: These medications can temporarily reduce pain, burning, and inflammation.
- Topical steroid creams: Mild cases of eczema can be treated with OTC steroid creams.
Prescription medications are often required to successfully treat symptoms of eczema and asthma. Common asthma treatments include:
Eczema is also treated with prescription medications. These can include:
- Topicals: These medications are applied directly to your affected skin. In addition to prescription steroid creams containing higher doses than OTC versions, topical calcineurin inhibitors and topical phosphodiesterase 4 inhibitors are also used to treat eczema. These medications block cells in your immune system that cause your symptoms.
- Oral steroids: For severe cases of eczema, your doctor might also prescribe oral steroids to decrease inflammation.
Autoimmunity In Atopic Dermatitis
- Division of Immunodermatology and Allergy Research, Department of Dermatology and Allergy, Hannover Medical School, Hanover, Germany
Atopic dermatitis , one of the most frequent inflammatory skin diseases worldwide, is believed to result from a disturbed skin barrier as well as aberrant immune reactions against per se harmless allergens. Starting mostly during childhood with a chronic, remitting relapsing course, the disease can persist into adulthood in about one fifth of patients. Immune reactions to self-proteins have been observed in AD patients already in the beginning of the Twentieth century, when human cellular extracts were shown to provoke skin lesions. However, the term autoimmunity has never been claimed, since AD is first and foremost an atopic disease. In contrast, this IgE-hallmarked autoreactivity was termed autoallergy and is ongoing discussed regarding its impact on the disease. Since severely affected patients tend to develop IgE-hypersensitivity reactions to numerous environmental allergens, the impact of immune responses to self-proteins is difficult to determine. On the other hand: any autoreactivity, irrespective of the magnitude, implicates the potential of driving the chronification of the disease while shaping the immune response. This review article revisits the observations made on autoallergy from an actual point of view and tries to approach the question whether these still point to a contribution to the disease.
Also Check: What To Use For Eczema On Eyelids
How Is Atopic Dermatitis Diagnosed
Your healthcare provider will ask about your health history and whether you have allergies or asthma. He or she will also ask about any family history of dermatitis, allergies, or asthma.
A healthcare provider can often diagnose atopic dermatitis by examining your skin. You may also have a patch test. This is used to find allergies by placing small amounts of allergens on the skin and watching for a response. A skin biopsy may also be done to rule out other causes of the rash.
How Is Dyshidrotic Eczema Diagnosed
You may be diagnosed by a general healthcare provider or a dermatologist. A dermatologist is a healthcare provider who specializes in diseases of the skin.
Your healthcare provider will ask about your medical history and your symptoms. Tell him or her about contact youve had to possible irritants. You will also have a physical exam. Your healthcare provider will need to make sure your symptoms arent caused by other conditions. These may include allergic contact dermatitis, ringworm, herpes, or a rare autoimmune disease. You may also have tests such as:
- Skin scraping or biopsy, to check for infection
- Patch skin testing, to look for allergic causes
- Blood tests, to check for an autoimmune cause
Don’t Miss: Best Thing For Toddler Eczema
Association Between Ad And Crohns Disease
Pooling result of five studies estimated an elevated prevalence of Crohns disease in AD compared to controls, with an average OR of 1.66 . Three cohort studies further detected an increased incidence of Crohns disease in AD, with a pooled RR of 1.38 , indicating that patients with AD had higher risk of developing Crohns disease .
What Can I Expect If Ive Been Diagnosed With Eczema
Nearly half of children with eczema will outgrow the condition or experience great improvement by the time they reach puberty. Others will continue to have some form of the disease. For adults with eczema, the disease can be generally well-managed with good skin care and treatment, although flare-ups of symptoms can occur throughout life.
Also Check: Que Es Eczema En Las Manos
Subacute Cutaneous Lupus Erythematosus
Subacute cutaneous lupus erythematosus is a form of lupus skin disease that is made worse by exposure to sunlight or artificial sources of ultraviolet radiation and does not produce scarring. It produces scaly red patches on the skin that can simulate the appearance of psoriasis occurring in sun-exposed areas of the body.
Patients with this form of skin lupus have a somewhat higher risk for developing the more severe internal complications of systemic lupus erythematosus compared to another common form of lupus skin disease named discoid lupus erythematosus.
Autoreactive T Cell Receptors A Matter Of Specificity
MHC-multimers are further tools to investigate the question whether a certain epitope is recognized by T cells. These multimerized, labeled MHC/peptide-complexes have been shown to bind to matching T cells with strong specificity, allowing their enumeration and characterization . With MHC class I-multimers harboring -NAC/Hom s2 epitopes, we observed specific staining of a subgroup of CD8+ T cells in patients that displayed detectable levels of specific IgE . This T cell fraction showed specific characteristics of effector/memory of terminally differentiated effector T cells, arguing for a contribution in an ongoing inflammatory process. Measuring cytokines secreted by these cells, we detected first of all IL-4, and further IFN-. While this phenotype, also termed Tc2, is relatively uncommon in healthy donors, it reflects the cytokine milieu in AD. Again, quality and quantity of the immune response suggest a contribution to the disease pathogenesis.
Also Check: Eczema Vs Psoriasis On Face
Impact Of Hereditary Status And Smoking
We identified a subgroup of 92 290 cases with information available on autoimmune diseases among biological parents. In multivariable analyses, adjusting for any parental autoimmune disease, the association between AD and any autoimmune disease remained stable . Further, the estimates remained stable after adjustment for diagnosis-specific parentoffspring associations when studying 15 of the most common autoimmune diseases .
In a subanalysis of 32 797 pregnant women with AD, registered in antenatal care during 19822016, the associations between AD and autoimmune dermatological diseases, gastrointestinal and rheumatological diseases, and MS remained stable in the multivariable analyses after adjustment for smoking .
How Soon Will We See New Eczema Treatments
Guttman-Yasskys study shows that abnormalities in the skin and the immune system in people with atopic dermatitis can be reversed by drugs that target just IL-4 and IL-13.
As a result of this new research, in November, the Food and Drug Administration granted dupilumab a breakthrough therapy designation. This designation may speed up the FDAs approval of the drug as a treatment for moderate-to-severe AD in adults.
Guttman-Yassky noted that its difficult to say how long phase III, or late stage, studies will take to complete. However, she said, We will probably see new drugs available to treat atopic dermatitis in the next few years.
Current treatments for AD include topical moisturizers, creams, soaps, and steroid ointments. Sunlight and even ultraviolet light therapy may also help.
Dr. Daniel Aires, director of dermatology at the University of Kansas Hospital, gave his thumbs-up to the new study. Aires told Healthline, The new drug appears to help normalize the atopic molecular signature Extremely severe disease can require systemic treatment, but these often bring risk of serious side effects. Dupilumab may be an important new modality for treating these patients. Longer term studies and aftermarket evaluation will be needed to assess longer term safety issues.
Recommended Reading: Hand Foot Mouth With Eczema